DOI: https://doi.org/10.1038/s41467-025-58362-9
Authors: Isaac Shiri, Giovanni Baj, Pooya Mohammadi Kazaj, Matthias R. Bigler, Anselm W. Stark, Waldo Valenzuela, Ryota Kakizaki, Matthias Siepe, Stephan Windecker, Lorenz Räber, Andreas A. Giannopoulos, George C. M. Siontis, Ronny R. Buechel, Christoph Gräni
Summary: This study developed a fully automated AI system that detects anomalous coronary artery origins in CT scans with over 99% accuracy, classifies their anatomical risk, and can alert clinicians to potentially life-threatening cases that might otherwise be missed.
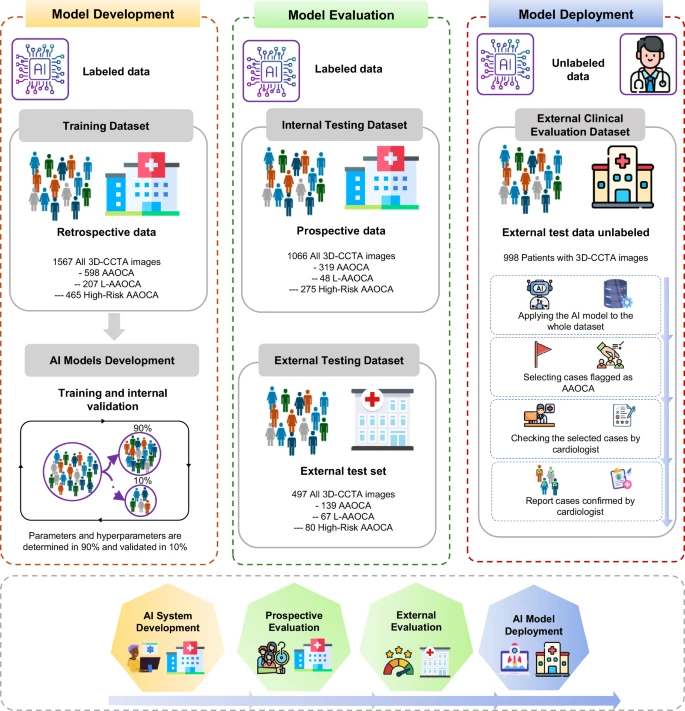
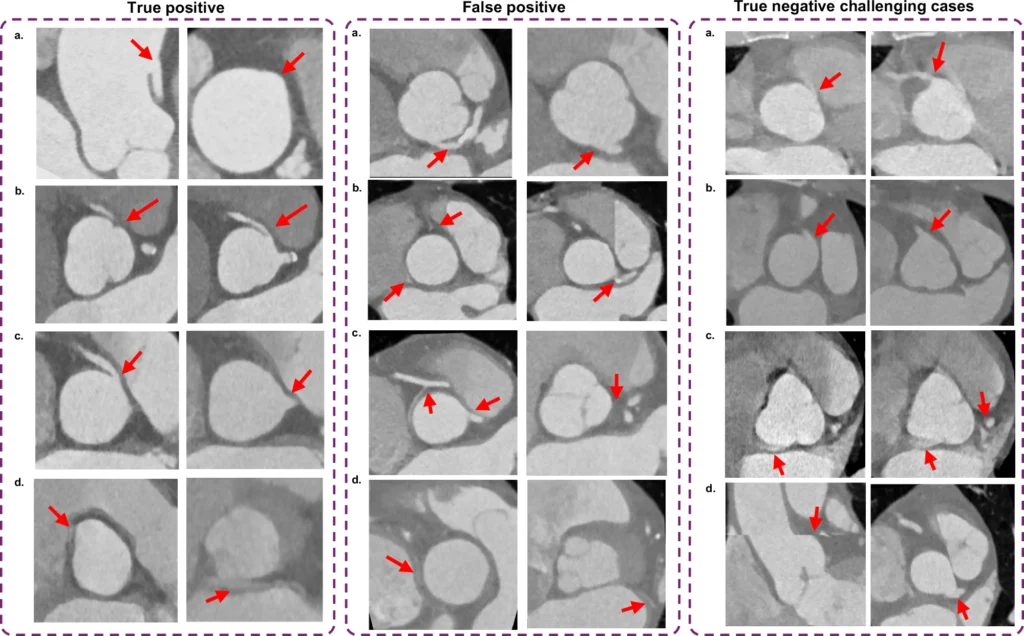
Anomalous aortic origin of the coronary artery (AAOCA) is a rare cardiac condition that can lead to ischemia or sudden cardiac death, yet it is often overlooked or falsely classified in routine coronary CT angiography (CCTA). Here, we developed, validated, externally tested, and clinically evaluated a fully automated artificial intelligence (AI)-based tool for detecting and classifying AAOCA in 3D-CCTA images. The discriminatory performance of the different models achieved an AUC ≥ 0.99, with sensitivity and specificity ranging 0.95-0.99 across all internal and external testing datasets. Here, we present an AI-based model that enables fully automated and accurate detection and classification of AAOCA, with the potential for seamless integration into clinical workflows. The tool can deliver real-time alerts for potentially high-risk AAOCA anatomies, while also enabling the analysis of large 3D-CCTA cohorts. This will support a deeper understanding of the risks associated with this rare condition and contribute to improving its future management.